Indications for Liver Ultrasound
Liver ultrasound is commonly utilized in the evaluation of various hepatic conditions. The most frequent indications include:
- 1. Monitoring chronic liver disease
- 2. Hepatocellular Carcinoma (HCC) Surveillance
- 3. Evaluation of Jaundice
- 4. Guidance for Interventional Procedures
- 5. Doppler Evaluation of Hepatic and Portal Circulation
- 6. Right Upper Quadrant (RUQ) Pain
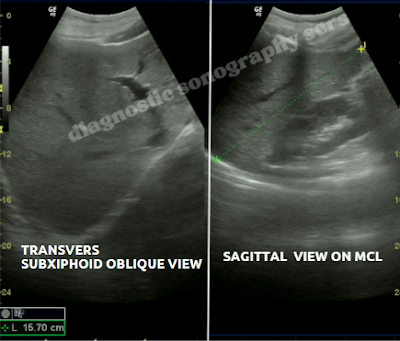
- 7. Pre- and Post-Liver Transplant Evaluation
- 8. Hepatomegaly or Splenomegaly
- 9. Suspected Liver Infection
- 10. Fatty Liver Disease (Hepatic Steatosis)
- 11. Detection and Evaluation of Liver Masses
- 12. Abnormal Liver Function Tests
1. Monitoring Chronic Liver Disease
Chronic liver disease refers to progressive deterioration of liver function over time, typically due to long-term inflammation, fibrosis, and eventual cirrhosis. Common causes include viral hepatitis (B and C), alcohol-related liver disease, non-alcoholic fatty liver disease (NAFLD), autoimmune hepatitis, and genetic/metabolic disorders.
Goals of Monitoring
- Assess disease progression
- Identify complications early
- Evaluate response to treatment
- Detect hepatocellular carcinoma (HCC) early
- Determine timing for interventions (e.g., transplant referral)
1. Clinical Assessment
Evaluation of symptoms: fatigue, jaundice, ascites, encephalopathy, GI bleeding.
Physical exam: hepatomegaly, splenomegaly, spider angiomas, edema, asterixis.
2. Laboratory Monitoring
- Liver Function Tests (LFTs): ALT, AST, ALP, GGT, bilirubin
- Synthetic Function: Albumin, INR/PT
- Complete Blood Count (CBC): Thrombocytopenia may indicate portal hypertension
- Renal Function: Important in advanced liver disease (e.g., hepatorenal syndrome)
- Alpha-fetoprotein (AFP): For HCC surveillance
3. Imaging Surveillance
- Ultrasound (every 6 months): Monitoring liver morphology, ascites, HCC screening
- Elastography (FibroScan): For fibrosis assessment
- CT or MRI: When ultrasound is inconclusive
4. Endoscopy
Upper GI endoscopy: To screen for esophageal varices in cirrhotics
5. Lifestyle and Comorbidity Management
- Alcohol cessation, weight loss, diabetes control
- Vaccinations: Hepatitis A and B, pneumococcus, influenza
- Nutritional support and vitamin supplementation
6. Treatment Response
- Viral load monitoring in hepatitis B/C
- ALT normalization in NAFLD after lifestyle changes
Complication Surveillance
- Ascites: Detected by exam and ultrasound. Perform paracentesis if needed.
- SBP: Suspect with worsening ascites. PMN ≥250/mm³ diagnostic.
- Hepatic Encephalopathy: Assessed clinically. Serum ammonia may help.
- HCC: Screen every 6 months with ultrasound ± AFP in high-risk patients.
Frequency of Follow-Up
- Compensated cirrhosis: Follow-up every 6–12 months
- Decompensated cirrhosis: Every 1–3 months
- High-risk HCC patients: Liver ultrasound every 6 months
2. Hepatocellular Carcinoma (HCC) Surveillance
HCC is the most common primary liver cancer, often arising in chronic liver disease. Surveillance aims to detect cancer early in high-risk patients.
Rationale
- Early-stage HCC is asymptomatic and treatable.
- Surveillance allows curative treatment: surgery, transplantation, or ablation.
- Improves survival by enabling early detection.
High-Risk Groups
- All cirrhotic patients
- Chronic hepatitis B (even without cirrhosis in certain demographics)
- Chronic hepatitis C with fibrosis or cirrhosis
- NASH with cirrhosis
- Autoimmune hepatitis, PBC, hemochromatosis with cirrhosis
Surveillance Approach
- Ultrasound every 6 months
- ± Serum AFP for enhanced sensitivity
- CT/MRI for poor ultrasound window or indeterminate lesions
Limitations
- Operator- and patient-dependent sensitivity
- Reduced detection for small/infiltrative tumors
- AFP is non-specific
Management of Findings
- Lesions ≥1 cm → CT/MRI evaluation
- < 1 cm → repeat US in 3 months
- Typical imaging may obviate biopsy
3. Evaluation of Jaundice
- Distinguish intrahepatic vs extrahepatic causes.
- Intrahepatic: altered liver texture, cirrhosis, hepatitis.
- Extrahepatic: bile duct dilatation from stones, strictures, or masses.
- Measure CBD diameter, assess for obstruction.
- Guide MRCP/ERCP when needed.
4. Guidance for Interventional Procedures
- Liver Biopsy: Real-time needle guidance
- Abscess Drainage: Ensures accurate catheter placement
- Cyst/Tumor Aspiration: Supports FNA procedures
- Tumor Ablation: RFA/MWA requires precise targeting
- Portal Vein Access: Used in TIPS procedures
5. Doppler Evaluation of Hepatic and Portal Circulation
- Blood Flow Assessment: Hepatic artery, portal vein, hepatic veins
- Portal Hypertension: Reduced portal velocity, reversal of flow, varices
- Portal Vein Thrombosis: Detect absence or reduced flow
- Budd–Chiari Syndrome: Identify hepatic vein/IVC obstruction
- Transplant Evaluation: Monitor vascular patency pre- and post-op
6. Right Upper Quadrant (RUQ) Pain
- First-line assessment: Gallbladder, liver, bile ducts, and kidney.
- Gallbladder: Detects stones, wall thickening, pericholecystic fluid, Murphy's sign.
- Liver causes: Abscesses, cysts, tumors, or hepatomegaly.
- Biliary tree: Checks for intra- and extrahepatic duct dilation.
- Kidney: Identifies hydronephrosis or stones mimicking RUQ pain.
7. Pre‑ and Post‑Liver Transplant Evaluation
- Pre‑transplant: Evaluate liver morphology, detect HCC or thrombosis, check vascular anatomy.
- Vascular mapping: Doppler of hepatic artery, portal vein, and hepatic veins.
- Immediate post‑transplant: Monitor graft perfusion and detect early complications.
- Hepatic artery complications: Detect thrombosis or stenosis via resistance index and flow patterns.
- Portal/hepatic vein evaluation: Identify thrombosis or stenosis affecting graft function.
- Long-term: Follow graft health, biliary complications, rejection, or recurrence.
8. Hepatomegaly or Splenomegaly
- Hepatomegaly: Measures liver size, contour, echotexture, and detects masses.
- Texture changes: Bright liver = steatosis; coarse = fibrosis or cirrhosis; focal lesions indicate masses.
- Splenomegaly: Quantifies spleen size; checks texture; may reflect portal hypertension, hematologic issues, or infection.
- Portal assessment: Doppler evaluation of portal vein, flow direction, and signs of collaterals or hypertension.
- Monitoring: Serial ultrasound tracks changes post-treatment or in disease progression.
9. Suspected Liver Infection
- Infections include: Pyogenic or amoebic abscesses, hepatitis, fungal involvement.
- Ultrasound: Shows hypoechoic or complex lesions in abscesses; diffuse enlargement in hepatitis.
- Intervention: Guides abscess aspiration or drainage and specimen collection.
- Doppler: Checks for vascular invasion or thrombosis in and around lesion.
- Follow-up: Monitors treatment response and resolution or progression.
10. Fatty Liver Disease (Hepatic Steatosis)
- Definition: Accumulation of fat causes increased echogenicity of the liver.
- Appearance: Brighter liver and difficult vessel/diaphragm visualization in advanced cases.
- Significance: Tied to obesity, diabetes, metabolic syndrome, and alcohol use; may progress to NASH or cirrhosis.
- Ultrasound role: Screens and monitors fat accumulation.
- Limitations: Cannot quantify fat or differentiate simple vs NASH accurately.
11. Detection and Evaluation of Liver Masses
- Mass types: Benign (hemangiomas, focal nodular hyperplasia, cysts) and malignant (HCC, metastases).
- Ultrasound features: Cysts = anechoic; hemangiomas = hyperechoic; malignant = heterogeneous, irregular, vascular.
- Doppler: Assesses vascular patterns to differentiate lesions.
- Further imaging: CT/MRI recommended for lesions >1 cm or unclear.
- Biopsy guidance: Employed for histological confirmation if needed.
12. Abnormal Liver Function Tests (LFTs)
- Persistent LFT elevation: Ultrasound evaluates structural causes—steatosis, fibrosis, masses, bile duct dilation.
- Assess complications: Detects ascites, splenomegaly, posthepatic obstruction.
- Follow-up: Helps monitor disease progression or therapeutic response.
© 2025 Your Institution or Author Name









No comments:
Post a Comment