Nuchal Translucency (NT) Screening
1. Scanning technique-[Step-by-Step Scanning Technique]
- [Step-1.]: Patient Preparation.
- [Step-2.]: Transducer Placement.
- [Step-3.]: Aligning the Fetus in a True Mid-Sagittal Plane.
- [Step-4.]: Optimize the Image.
- [Step-5.]: Differentiation of Structures.
3. NB measuring method
4. Amniotic fluid volume measuring method
5. Anatomical Assessment of the Fetal Profile
6. Fronto-Maxillary Facial (FMF) Angle
7. Forehead-to-Nasal Tip Ratio
8. Grayscale-Based Fetal Malformations Detected During NT Screening
1. Tricuspid Valve Regurgitation
2. Ductus Venosus (DV) Doppler
3. Fetal Heart Rate (FHR)
4. Uterine artery Doppler
5. Role of Other Fetal Doppler Parameters
6. Doppler-Based Fetal Anomalies During NT Screening
- Maternal age.
- Biochemical markers
- Additional ultrasound markers (nasal bone, ductus venosus, tricuspid flow)
- The goal is to provide a risk estimate, not a diagnosis, and to help guide decisions for further testing like NIPT or invasive testing.
- Measures the fluid-filled space at the back of the fetal neck (NT).
- Increased NT is associated with:
- Trisomy 21 (Down syndrome)
- Trisomy 18 (Edwards syndrome)
- Trisomy 13 (Patau syndrome)
- Turner syndrome (Monosomy X)
- Enlarged NT may also indicate:
- Congenital heart defects
- Diaphragmatic hernia
- Body stalk anomaly
- Other syndromic conditions (e.g., Noonan syndrome)
- NT measurement is often combined with:
- Serum markers (PAPP-A, free β-hCG)
- Maternal age
- This combination improves the detection rate (>90%) for Down syndrome with a low false-positive rate (~5%).
- NT scan uses standard ultrasound—no radiation or risk to the fetus.
- Provides critical early information without invasive procedures.
- Abnormal NT results may prompt:
- Non-invasive prenatal testing (NIPT)
- Fetal echocardiography
- Chorionic villus sampling (CVS) or amniocentesis for genetic diagnosis
- Ask the mother to have a partially filled bladder (optional).
- Position her comfortably in the supine or slightly tilted position.
- Use a transabdominal probe (3.5–5 MHz).
- In early gestations or with unfavorable views, a transvaginal probe (5–9 MHz) may be used.
- Key anatomical landmarks:
- The fetal head and thorax must be in a neutral position (neither hyperextended nor flexed).
- The echogenic tip of the nose should be visible.
- The rectangular shape of the palate must be clearly seen.
- The translucent diencephalon and fourth ventricle (intracranial translucency) should be visible.
- Maternal Preparation: Empty bladder (if transvaginal), partially full bladder (if transabdominal).
- Probe Orientation: Align the transducer parallel to the fetal body axis.
- Adjusting Fetal Position: Use gentle abdominal pressure or ask the patient to change position.
- Zoom & Focus: Enlarge the image so that the fetal head and upper thorax occupy at least 75% of the screen.
- Off-axis images: May mimic the midline but lack key structures (e.g., missing nasal bone).
- Fetal movement: Wait for stillness or reattempt alignment.
- Incorrect flexion/extension: Identify and correct before measuring NT.
- Annotated ultrasound images showing:
- Diagrams highlighting critical landmarks
- Risk of inaccurate NT measurement
- False positives/negatives in screening for chromosomal abnormalities
- Zoom in until the fetal head and upper thorax fill at least 75% of the screen.
- Use grayscale only (do not use Doppler).
- Adjust gain and focus to enhance bony structures like the frontal bone.
- Amnion (the thin membrane surrounding the fetus),
- Fetal skin,
- Subcutaneous tissues,
- Umbilical cord if nearby.
- No Doppler,
- No color overlays,
- No power Doppler.
- Confirm gestational age,
- Establish the expected date of delivery (EDD),
- Determine if the fetus is within the 11–13+6 weeks window required for NT (Nuchal Translucency) screening,
- CRL is the distance from the top of the fetal head (crown) to the bottom of the trunk (rump).
- Grayscale imaging clearly displays:-
- a). The outer borders of the head and rump,
- b).Internal fetal structures (e.g., spine) for correct orientation.
- Ensures that only the fetal length is measured, excluding limbs or yolk sac.
- Grayscale contrast allows: Clear identification of the outer edge of the crown and outer edge of the rump.
- This minimizes error and improves reproducibility.
- NT screening is valid only when:- CRL is between 45 mm and 84 mm, roughly corresponding to 11–13+6 weeks.
- Grayscale imaging ensures that the fetus is scanned in a neutral position (not flexed or extended), giving a true CRL.
- Align the fetus in a true mid-sagittal plane, showing:
- Tip of the nose
- Nasal bone
- Palate
- Maxilla
- Mandible
- Forehead
- The fetus should be in a neutral position (not flexed or extended).
- Key landmark: The forehead appears as a smooth echogenic curve above the nasal bridge.
- No Doppler or color should be used.
- Ensures standardization across centers.
- The fetal skin line (outer border).
- The amniotic fluid (background).
- Proper magnification and mid-sagittal plane acquisition are easier with grayscale imaging.
Step-1. Patient Preparation
Why Structural Differentiation Matters:
Misidentification can lead to false-positive or false-negative risk assessments for chromosomal abnormalities.
Using grayscale imaging only for NT measurement:
Grayscale ultrasound plays a critical role in accurately measuring the Crown-Rump Length (CRL) during nuchal translucency (NT) screening. CRL is the most reliable parameter for dating early pregnancy and for determining eligibility and reference ranges for NT measurement (which must be done between CRL 45–84 mm).
Key Roles of Grayscale Imaging
1. Optimal Visualization of Fetal AnatomyHow Nuchal Translucency (NT) is Measured
Step-1: Preparation for the Scan
No special preparation is needed, but a full bladder may help improve image clarity.
The scan is typically abdominal, but in some cases, a transvaginal ultrasound may be used for better visualization.
Step-2: Performing the Ultrasound
The sonographer places an ultrasound probe on your abdomen (or inserts a transvaginal probe if necessary).
The image is magnified to ensure accurate measurement.
Step-3: Measuring the Nuchal Translucency
The sonographer identifies the fluid-filled space at the back of the baby’s neck.
Using calipers, the maximum thickness of this translucent (fluid-filled) area is measured.
The measurement is taken three times, and the largest reading is recorded for accuracy.
Step-4: Interpreting the NT Measurement
Increased NT thickness: Over 3.5 mm may indicate a higher risk of chromosomal abnormalities like Down syndrome (Trisomy 21), Trisomy 18, or congenital heart defects.
Next Step:
This combined screening helps determine if further diagnostic testing (e.g., NIPT, CVS, or amniocentesis) is recommended.
If the NT is increased, further testing (such as NIPT, CVS, or amniocentesis) may be recommended.
Nasal Bone (NB) Measuring Method During NT Screening
Normal range of NB
| CRL (mm) | Expected NB Length (mean ± SD) |
|---|---|
| 45–54 mm | ~1.4 mm (range: 1.1–1.8 mm) |
| 55–64 mm | ~1.7 mm (range: 1.3–2.1 mm) |
| 65–74 mm | ~1.9 mm (range: 1.5–2.3 mm) |
| 75–84 mm | ~2.1 mm (range: 1.7–2.5 mm) |
- Plane:- True mid-sagittal view of the fetal profile (same as NT view)
- Fetal:- Position Head in neutral position, no flexion or hyperextension
- Zoom:- Fetal head and upper thorax should occupy at least 75% of the image
- Magnification:- Maximize to clearly visualize nasal bridge and skin
- Image Quality:- High-resolution grayscale with appropriate gain (to avoid under/overexposing bones)
- Skin line (top)
- Nasal bone (middle, shorter and more echogenic)
- Tip of the nose (hard palate or nasal tip) (bottom)
Amniotic fluid volume (AFV) is not routinely measured quantitatively as part of the screening. However, qualitative assessment of amniotic fluid is still done, and significant abnormalities may be noted.
Points about AFV during NT Screening:
1. Amniotic Fluid Volume Evaluation:
- Not measured using AFI (Amniotic Fluid Index) or MVP (Maximum Vertical Pocket) this early.
- Subjective/qualitative assessment is typically performed:
- Sonographer ensures adequate amniotic fluid surrounds the fetus.
- Significant findings like oligohydramnios (too little fluid) or polyhydramnios (too much fluid) are reported if noted.
- Usually starts around 20 weeks during the anomaly scan.
- Measured using:
- AFI in a four-quadrant technique (second and third trimesters).
- MVP method, especially in twin pregnancies.
- Abnormal fluid volume in the first trimester is rare but, if present, may indicate:
- Early rupture of membranes (very rare).
- Fetal anomalies.
- Chromosomal abnormalities.
1. 3D Volume Acquisition:
- Use a 3D transducer to capture a full volume of the amniotic sac.
- Usually performed in a transabdominal or transvaginal scan depending on fetal position.
- Most common method for 3D volume measurement.
- Steps:
- Freeze the volume image.
- Outline the amniotic fluid manually or semi-automatically on rotating planes (every 15° or 30°).
- The software reconstructs a 3D volume.
- The calculated fluid volume is displayed in milliliters (mL).
- ome studies propose normal ranges by gestational week, but these are not yet standardized for clinical use.
| Gestational Age (weeks) | Mean 3D AFV (mL) |
|---|---|
| 11 weeks | ~30–35 mL |
| 12 weeks | ~40–50 mL |
| 13 weeks | ~60–70 mL |
Note: TIn rare cases of suspected abnormalities, a follow-up scan and further investigations are recommended to monitor evolving fluid dynamics.
What is the Fetal Profile?
- Forehead
- Nasal bone
- Nasal tip
- Nasal tip
- Upper and lower lips
- Maxilla and mandible
- Chin (mentum)
- Flattened forehead or Vertical, or bulging forehead: Trisomy 21 or Early signs of syndromes
- Ensure neutral fetal position: Prevent measurement and shape distortion.
- Optimize grayscale settings: Clear visualization of frontal bone and contour.
- Definition: Angle between the line along the upper surface of the maxilla and the line along the frontal bone.
- Mid-sagittal view of the face
- One line: along the upper aspect of the maxilla
- Second line: tangential to the frontal bone
- Measure the angle between these two lines
- Forehead length: From the leading edge of the frontal bone to the nasion (root of the nose).
- Nasal tip length: From the nasion to the nasal tip.
- Forehead-to-Nasal Tip Ratio = Forehead Length / Nasal Tip Length
- Alobar holoprosencephaly
- Semilobar holoprosencephaly
- Lobar Holoprosencephaly
- Meningocele
- Encephalocele
- Meningoencephalocystocele
- Median cleft
- Unilateral (Upper) cleft lip (CL/±P)
- Unilateral (Lower) cleft lip (CL/±P)
- Bilateral cleft lip (CL/±P)
- Obtain an apical four-chamber view of the fetal heart using color Doppler.
- Ensure the fetus is still and the heart rate is between 120–160 bpm.
- Use a small Doppler gate (<2 b="" mm="">) over the tricuspid valve.
- TR is identified as a reverse flow jet into the right atrium during systole.
- Normal (No TR): No significant reverse jet seen during systole
- Abnormal (TR Present): Reverse jet lasting ≥ half of systole with velocity ≥ 60 cm/s
- Presence of TR is associated with:
- Trisomy 21
- Trisomy 18
- Congenital heart defects
- Used in conjunction with NT, nasal bone assessment, and biochemical markers to refine risk calculation.
Fronto-Maxillary Facial (FMF) Angle
It is a craniofacial ratio calculated on a mid-sagittal plane ultrasound image, using two linear measurements:
1. Acrania
2. Anencephaly
3. Holoprosencephaly
7. Cystic hygroma
8. Spina bifida
9. Ectopia cordis
10. Omphalocele
11. Gastroschisis
12. Megacystis
13. Clubfoot
14. Polydactyly
15. Anasarca (Skin edema)
16. Pericardial effusions
17. Pleural effusions
18. Ascites
Findings
📄 Report Sample Line– Acrania (During First Trimester / NT Screening)
Absence of calvarial bones with disorganized brain tissue consistent with acrania, noted on gray scale imaging. Findings suggest a lethal neural tube defect.
Conclusion
📋 Features are consistent with acrania (A lethal neural tube defect).
Recommendation:
Early referral to a fetal medicine specialist is advised.
Recommend detailed follow-up anomaly scan and genetic counseling.
Findings
📄 Report Sample Line– Anencephaly (During First Trimester / NT Screening)
There is absence of the cranial vault with exposed brain tissue ("frog-eye" appearance). The cerebral hemispheres are not covered by bone, and the cranial contour above the orbits is not visualized. This is consistent with a severe neural tube defect.
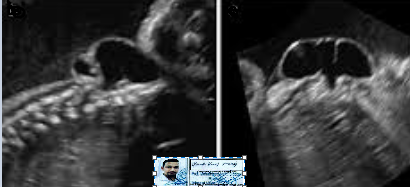
Fig-1
Fig-2
Conclusion
📋 Sonographic findings are consistent with Anencephaly (A lethal neural tube defect).
Recommendation:
Early referral to a fetal medicine specialist is advised
Recommend detailed follow-up anomaly scan and genetic counseling or 3D/4D Snan.
Findings
📄 Report Sample Line– Alobar holoprosencephaly (During First Trimester / NT Screening)
Gray scale imaging of a fetal brain showing a monoventricular brain cavity with absence of midline falx, fused thalami, and distorted craniofacial structures, suggestive of alobar holoprosencephaly.
Conclusion
📋 Sonographic features are highly suggestive of holoprosencephaly, most consistent with the alobar form, a severe and lethal forebrain malformation.
Recommendation:
Recommend urgent referral to fetal medicine specialist for detailed neurosonography and genetic counseling. Karyotyping or chromosomal microarray testing is advised to assess for associated anomalies such as trisomy 13.
Note: Associated facial anomalies (e.g., hypotelorism, proboscis) may also be present.
Findings
Type-2: Semilobar holoprosencephaly
📄 Report Sample Line– Semilobar holoprosencephaly (During First Trimester / NT Screening)
Gray scale imaging ofa fetal brain showing a partial separation of the cerebral hemispheres posteriorly, with a single ventricular cavity anteriorly, partially formed falx cerebri, and incomplete division of the thalami, consistent with semilobar holoprosencephaly.
Conclusion
📋 Sonographic features are highly suggestive of holoprosencephaly, most consistent with the semilobar a moderate form of forebrain malformation with significant neurodevelopmental implications.
Recommendation:
Recommend urgent referral to fetal medicine specialist for detailed neurosonography and genetic counseling. Karyotyping or chromosomal microarray testing is advised to assess for associated anomalies such as trisomy 13.
Note: Subtle midline facial anomalies such as hypotelorism may also be noted.
Findings
Type-1: Lobar holoprosencephaly
📄 Report Sample Line– Lobar Holoprosencephaly (During First Trimester / NT Screening)
Gray scale imaging of a fetal brain showing near-complete separation of cerebral hemispheres, with subtle fusion of the frontal lobes, presence of an interhemispheric fissure and falx cerebri, and a mildly abnormal configuration of the frontal horns, suggestive of lobar holoprosencephaly.
Conclusion
📋 Imaging findings are consistent with lobar holoprosencephaly, the mildest form of forebrain malformation, which may still be associated with neurodevelopmental delay and chromosomal anomalies.
Recommendation:
Recommend referral to a fetal medicine specialist for detailed neurosonography and genetic counseling. Fetal MRI and genetic testing (including karyotyping or chromosomal microarray) are advised to evaluate associated anomalies and assist in prognostic assessment.
Note: Facial anomalies may be minimal or absent.
Findings
📄 Report Sample Line– Cephalocele/Meningocele (During First Trimester / NT Screening)
Gray scale imaging of a fetal brain showing a midline extracranial cystic mass extending through a defect in the occipital skull region, consistent with a cephalocele. The intracranial structures appear disrupted at the site of the lesion.
Conclusion
📋 Sonographic features are suggestive of a cephalocele/Meningocele a neural tube defect involving herniation of intracranial contents through a skull defect, most commonly occipital
Recommendation:
Recommend urgent referral to fetal medicine for detailed neurosonography and assessment for associated anomalies, including evaluation for Meckel–Gruber syndrome and chromosomal abnormalities. Karyotyping or chromosomal microarray and follow-up imaging including fetal MRI are advised for prognostic and counseling purposes.
Findings
📄 Report Sample Line– Cephalocele/Encephalocele (During First Trimester / NT Screening)
Gray scale imaging of a fetal brain showing a midline occipital bony defect with herniation of intracranial brain tissue into a well-defined extracranial mass, consistent with an encephalocele. The cranial vault appears abnormal posteriorly, and the intracranial anatomy is disrupted at the lesion site..
Conclusion
📋 Sonographic features are consistent with an cephalocele/encephalocele a type of neural tube defect characterized by herniation of brain tissue through a skull defect.
Recommendation:
Follow-up with fetal MRI.
Findings
📄 Report Sample Line– Cephalocele/Meningo-encephalocele (During First Trimester / NT Screening)
Gray scale imaging of a fetal brain showing a posterior skull defect with a complex extracranial mass containing meninges, brain tissue, and an anechoic component suggestive of a dilated ventricular structure, consistent with a meningoencephalocystocele. There is discontinuity of the calvarium in the occipital region, and distortion of intracranial anatomy.
Conclusion
📋 Features are consistent with a Meningo-encephalocele a severe form of cephalocele involving herniation of meninges, brain tissue, and part of the ventricular system through a skull defect.
Recommendation:
Consider second-trimester fetal MRI and multidisciplinary counseling regarding.
Findings
📄 Report Sample Line– Median cleft (During First Trimester / NT Screening)
A median facial cleft is noted, characterized by abnormal discontinuity of the midline upper lip and/or premaxillary region on coronal facial view. Nasal bone visualization may be suboptimal.
Conclusion
📋 Findings are suggestive of a median facial cleft anomaly which may be associated with underlying syndromic or chromosomal abnormalities.
Recommendation:
Recommend a targeted Level II anomaly scan, fetal echocardiography, and genetic counseling. Consider karyotyping and/or chromosomal microarray testing. 3D ultrasound and fetal MRI may aid in further anatomical assessment.
Findings
📄 Report Sample Line– Unilateral (Upper) cleft lip (CL/±P) (During First Trimester / NT Screening)
Shows a unilateral upper cleft lip noted on coronal facial view — defect visualized on the [left/right] side of the upper lip with discontinuity in the soft tissue line.
Conclusion
📋 Findings suggest the presence of a unilateral cleft lip. Detailed evaluation of the maxilla and palate is limited at this gestational age
Recommendation:
Recommend follow-up with a targeted anomaly scan around 18–22 weeks for detailed assessment of the lip and palate. 3D/4D ultrasound and genetic counseling are advised.
Findings
📄 Report Sample Line– Unilateral (Lower) cleft lip (CL/±P) (During First Trimester / NT Screening)
shows a unilateral lower cleft lip identified on coronal facial view during NT screening. Defect noted on the [left/right] side of the lower lip, with possible involvement of the lower alveolar ridge.
Conclusion
📋 Findings are suggestive of a unilateral lower cleft lip (CL)
Recommendation:
Detailed follow-up with mid-trimester targeted anomaly scan and 3D facial imaging is recommended.
Findings
📄 Report Sample Line– Bilateral cleft lip (CL/±P) (During First Trimester / NT Screening)
Bilateral discontinuity of the upper lip visualized on coronal facial views during first-trimester NT screening, suggestive of bilateral cleft lip.
Note:-Palatal involvement (cleft lip with or without palate involvement – CL/±P) cannot be confidently assessed at this stage.
Conclusion
📋 Sonographic features are suspicious for bilateral cleft lip with possible extension to the alveolus and/or palate. Sonographic features are suspicious for bilateral cleft lip, with possible extension to the alveolus and/or palate.
Recommendation:
Advise follow-up with a detailed second-trimester anomaly scan and 3D facial ultrasound to confirm the extent of the defect
Findings
📄 Report Sample Line– Absent nasal bone(During First Trimester / NT Screening)
Nasal bone not visualized in the mid-sagittal view. Considered to absent nosal bone.
Conclusion
📋 Absent nasal bone is a significant soft marker associated with an increased risk of aneuploidies, particularly Trisomy 21, Trisomy 18, and Trisomy 13
Recommendation:
Recommend comprehensive risk assessment including nuchal translucency (NT) measurement, maternal serum screening (PAPP-A, free β-hCG).
Findings
📄 Report Sample Line- Cystic hygroma (During First Trimester / NT Screening)
Septated fluid-filled cystic structure noted at the posterior fetal neck region during first-trimester NT scan, consistent with cystic hygroma. Lesion appears multiloculated and extends bilaterally.
Conclusion
📋 Sonographic features are indicative of a cystic hygroma.
Recommendation:
Recommend prompt referral for genetic counseling and offer diagnostic testing (chorionic villus sampling or amniocentesis). Detailed early fetal echocardiography and follow-up anomaly scan are advised.
Findings
📄 Report Sample Line- Spina bifida (During First Trimester / NT Screening)
shows an open neural tube defect (spina bifida) noted in the lumbosacral region, with splaying of posterior ossification centers.
Conclusion
📋 Findings suggest a spina bifida.
Recommendation:
Follow-up with detailed fetal anomaly scan, fetal echocardiography, and multidisciplinary evaluation is advised
Findings
📄 Report Sample Line- Ectopia cordis (During First Trimester / NT Screening)
The fetal heart is visualized partially/completely outside the thoracic cavity on anterior chest wall, consistent with ectopia cordis. There is a midline thoracic wall defect with abnormal cardiac position and motion outside the thorax.
Conclusion
📋 Sonographic findings are diagnostic of ectopia cordis.
Recommendation:
follow-up MRI
Findings
📄 Report Sample Line- Omphalocele (First Trimester / NT Screening)
Midline anterior abdominal wall defect noted at the base of the umbilical cord insertion, containing herniated bowel and/or liver within a membranous sac consistent with omphalocele. Umbilical cord is seen inserting into the apex of the sac.
Conclusion
📋 Findings are suggestive of Omphalocele.
Recommendation:
Further evaluation with detailed anomaly scan and fetal echocardiography.
Findings
📄 Report Sample Line- Gastroschisis (During First Trimester / NT Screening)
Paraumbilical right-sided abdominal wall defect identified, with free-floating bowel loops herniating directly into the amniotic cavity without a surrounding membrane. The umbilical cord inserts normally adjacent to the defect.
Conclusion
📋 Sonographic features are diagnostic of Gastroschisi
Recommendation:
Follow-up with serial growth scans and assessment of bowel appearance.
Findings
📄 Report Sample Line- Megacystis (During First Trimester / NT Screening)
Significantly enlarged fetal urinary bladder observed. Measuring ≥7 mm in longitudinal diameter.
Conclusion
📋 Findings are consistent with Megacystis
Recommendation:
Follow-up with detailed anomaly scan.
Findings
📄 Report Sample Line- Clubfoot (During First Trimester / NT Screening)
Abnormal positioning of the fetal foot noted with persistent inward rotation and plantar flexion of the foot toward the tibia, consistent with unilateral/bilateral clubfoot. Long-axis views confirm fixed abnormal alignment.
Conclusion
📋 Sonographic findings are consistent with clubfoot (talipes equinovarus).
Recommendation:
Follow up fetal MRI.
Findings
📄 Report Sample Line- Polydactyly (During First Trimester / NT Screening)
Shows extra digit(s) visualized on the fetal hand/foot (specify: preaxial/postaxial, unilateral/bilateral) during detailed limb evaluation. Sonographic findings are consistent with polydactyly.
Conclusion
📋 Sonographic findings are consistent with Polydactyly
Recommendation:
Follow-up 4D scan.
Findings
📄 Report Sample Line- Anasarca (During First Trimester / NT Screening)
Diffuse subcutaneous soft tissue thickening with generalized skin edema (>5 mm) observed across the fetal body.
Conclusion
📋 Sonographic features are indicative of fetal anasarca a manifestation of hydrops fetalis
Recommendation:
Detailed fetal echocardiography
TORCH screening
MCA Doppler for fetal anemia
Karyotyping (amniocentesis)
Nots:Possible etiologies include cardiac anomalies, chromosomal abnormalities, fetal anemia, infections (e.g., Parvovirus B19), or lymphatic dysplasia. Prognosis depends on the underlying cause and severity.
Findings
📄 Report Sample Line- Pericardial effusions (During First Trimester / NT Screening)
Anechoic fluid collection noted in the pericardial space, surrounding the fetal heart, measuring approximately __ mm in thickness. Effusion is symmetric and persists throughout the cardiac cycle. No signs of cardiac tamponade observed at this stage.
Conclusion
📋 Sonographic finding of fetal pericardial effusion.
Recommendation:
Follow-up ultrasound for effusion monitoring.
Findings
📄 Report Sample Line- Pleural effusions (During First Trimester / NT Screening)
Anechoic fluid collections noted within the fetal thoracic cavity, located between the lung and chest wall, consistent with unilateral/bilateral pleural effusion.
Conclusion
📋 Sonographic findings are consistent with fetal pleural effusion.
Recommendation:
Screen for TORCH infections and fetal anemia (MCA Doppler).
Findings
📄 Report Sample Line- Ascites (During First Trimester / NT Screening)
Anechoic free fluid visualized within the fetal peritoneal cavity, outlining bowel loops and liver contours, consistent with fetal ascites. No associated bowel wall thickening or echogenicity noted at this stage.
Conclusion
📋 Sonographic features indicate fetal ascites.
Recommendation:
Screen for fetal infections (TORCH, Parvovirus B19), and assess fetal heart and urinary tract.
Note:-Fetal early sign of hydrops fetalis or secondary to intra-abdominal pathology, infections, genitourinary obstruction, cardiac failure, or chromosomal abnormalities.
Findings
📄 Report Sample 00 (First Trimester / NT Screening)
00
Conclusion
📋 00
Recommendation:
00
| System/Area | Possible Malformation(s) | Grayscale Clues |
|---|---|---|
| Cranial/Brain | Acrania/Anencephaly, Holoprosencephaly, Cephalocele | Absent cranial vault, single cerebral ventricle, extracranial mass |
| Face | Facial clefts, Absent nasal bone | Discontinuity in facial contour, hypoplastic/absent echogenic nasal bone |
| Neck | Cystic hygroma | Large septated fluid collection at the nuchal region |
| Spine | Spina bifida | Irregular or open spinal contour, posterior defect |
| Thorax/Heart | Cardiac anomalies, Ectopia cordis | Abnormal cardiac axis/position, heart outside thorax |
| Abdomen | Omphalocele, Gastroschisis | Herniation at base of umbilical cord (membrane-covered or not) |
| Urinary Tract | Megacystis | Bladder diameter ≥7 mm (longitudinal) in 11–14 weeks |
| Limb/Extremities | Limb reduction defects, Clubfoot, Polydactyly | Absent, short, or abnormally angled limbs or digits |
| Hydrops | Non-immune hydrops | Skin edema, pericardial/pleural effusions, ascites |
The Forehead-to-Nasal Tip Ratio is a relatively rarely used soft marker assessed during first-trimester nuchal translucency (NT) screening,
It is a craniofacial ratio calculated on a mid-sagittal plane ultrasound image, using two linear measurements:
TR assessment is performed during the 11–13 weeks + 6 days scan, especially in cases with increased NT or other risk indicators.
Technique:Note: TR alone is not diagnostic. It is a supplementary marker to be interpreted with other first-trimester screening results.
Below is a table of Doppler parameters used in Ductus Venosus assessment during 11–13+6 weeks gestation:
| Parameter | Measured Value | Normal Range / Interpretation |
|---|---|---|
| Ductus Venosus PI | 1.2 | < 95th percentile (~1.0–1.5 at 11–13w) |
| Ductus Venosus RI | 0.6 | 0.5 – 0.8 |
| Ductus Venosus PSV | 35 cm/s | 30 to 60 cm/s |
| Ductus Venosus A-wave | Positive | Forward flow (Normal) / Reversed or Absent (Abnormal) |
1. Indicator of Fetal Well-Being:
- 1. Normal FHR Values: Typically, the normal range in the first trimester is between 120–160 beats per minute. A normal heart rate suggests proper cardiac function and overall fetal health.
- Abnormal FHR: Deviations such as tachycardia (elevated FHR) or bradycardia (lower than normal FHR) can be indicators of potential fetal distress, congenital heart issues, or other underlying abnormalities.
- Confirmation of Fetal Viability: Recording the fetal heart rate confirms that the fetus is alive and supports the accurate measurement of NT.
- Guidance for Image Acquisition: A clear, consistent heart rate helps sonographers optimize the image quality and ensure that the measurements (including NT thickness) are taken when the fetus is in an optimal position.
While NT measurement is the main focus for chromosomal risk estimation, the inclusion of FHR provides additional physiological data. If there’s an abnormal heart rate along with an increased NT measurement, it may raise the suspicion for certain conditions (including cardiac anomalies) and prompt further investigation.
4. Indicator of Fetal Well-Being:Research has evaluated the correlation between abnormal FHR parameters and increased NT thickness. Although FHR is not directly incorporated into the NT risk calculation algorithms, variations in FHR might reinforce the clinical decision-making process when NT measurements are on the borderline.
5. Measurement and MethodologyFHR is most commonly measured using ultrasound modalities:
- Doppler Ultrasound:Utilizes the Doppler effect to detect the movement of blood in the fetal heart, providing an immediate reading of the FHR.
- M-Mode Ultrasound:Offers a graphical representation of the heart motion over time, which helps in verifying the heart rate and rhythm.
- The simultaneous recording of FHR and NT allows for a comprehensive assessment during the first-trimester scan. Proper ultrasound technique ensures the fetus is imaged in a neutral position without excessive movement, which is crucial for accurate NT measurement and reliable FHR determination.
Uterine artery Doppler assesses blood flow resistance in the uterine arteries, which supply the placenta. Abnormal flow patterns in the first trimester (11–14 weeks) can indicate impaired placentation, which may lead to complications like.
- Preeclampsia.
- Fetal Growth Restriction (FGR).
- Placental insufficiency.
In low-risk, asymptomatic pregnancies, uterine artery Doppler is not required during NT screening. The guideline that uterine artery Doppler is not required in low-risk, asymptomatic pregnancies during NT screening is widely accepted in international practice, including in regions like:
- United Kingdom – per NICE and Fetal Medicine Foundation (FMF) guidelines.
- United States – per ACOG (American College of Obstetricians and Gynecologists).
- Canada –per SOGC (Society of Obstetricians and Gynaecologists of Canada).
- Europe – following ISUOG (International Society of Ultrasound in Obstetrics and Gynecology).
- >Australia/New Zealand – per RANZCOG guidelines.
- History of preeclampsia or FGR
- Maternal conditions like hypertension, autoimmune disorders
- Abnormal serum markers (e.g., low PAPP-A)
- As part of combined screening models (e.g., Fetal Medicine Foundation risk algorithm)
In first-trimester screening, additional Doppler parameters support the evaluation of fetal cardiac function and placental health. Below is a summary of key Doppler indices and their relevance.
| Parameter | Role / Relevance | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ductus Venosus (DV) | Abnormal flow (reversed or absent A-wave) may indicate chromosomal anomalies, especially Trisomy 21, and fetal cardiac dysfunction. | ||||||||||||||||
| Tricuspid Regurgitation (TR) | Presence of TR during systole is linked with chromosomal defects (especially T21) and congenital heart disease (CHD). | ||||||||||||||||
| Uterine Artery PI | Elevated mean PI may indicate impaired placental perfusion, increased risk of preeclampsia and FGR (fetal growth restriction). | ||||||||||||||||
| Umbilical Artery PI | Less informative in the first trimester, but abnormal values could suggest early placental resistance or vascular pathology. | ||||||||||||||||
| Middle Cerebral Artery (MCA) PI | Usually reserved for second/third trimester, but early deviation may reflect cardiac output imbalance. Low PI (<5th br="" brain-sparing="" centile="" effect="" in="" iugr.=""> Normal range 1.3–2.0 (decreases with GA) High PSV >1.5 multiples of the median (MoM) may indicate fetal anemia (e.g., Rh isoimmunization).
|
||||||||||||||||
| Cerebroplacental Ratio (CPR) | Rarely used in first trimester; more valuable in third trimester to evaluate fetal oxygenation and reserve.CPR (Cerebroplacental Ratio)
|
If the Nuchal Translucency (NT) measurement is higher than normal (typically >3.5 mm), it does not mean the baby definitely has a problem, but it may indicate an increased risk for certain conditions.
Possible Implications of High NT
- Down syndrome (Trisomy 21)Edwards syndrome (Trisomy 18)
- Edwards syndrome (Trisomy 18)
- Patau syndrome (Trisomy 13)
- Turner syndrome (Monosomy X)
- Noonan syndrome
- Other single-gene disorders
- Miscarriage
- Fetal death
- Intrauterine growth restriction (IUGR)
Steps After High NT
2. First-Trimester Combined Screening (NT + PAPP-A + free β-hCG)
3. Non-invasive Prenatal Testing (NIPT) – analyzes fetal DNA in maternal blood
4. Diagnostic Testing (if indicated)
- Chorionic Villus Sampling (CVS) at 11–13 weeks
- Amniocentesis after 15 weeks
Although Oligohydramnios is more commonly evaluated in the second and third trimesters, a during the first trimester (11–13 weeks) may signal early complications.
Sonographic Clues:
- Fetus appears closely apposed to uterine wall.
- Inability to visualize adequate fluid around fetus.
- Compressed amniotic sac or oligoamnios-like pattern.
🧾 Possible Causes:
- Early rupture of membranes (PROM).
- Severe fetal renal anomalies (e.g., bilateral renal agenesis – rare this early).
- Placental insufficiency or poor perfusion.
- Chromosomal abnormalities (in association with other markers).
- Amniotic band syndrome.
Management / Follow-Up:
- Repeat scan within 1–2 weeks to assess fluid changes.
- Check for fetal heartbeat and anatomy.
- Evaluate for signs of membrane rupture.
- Consider referral for early fetal medicine consultation.
While Polyhydramnios is rarely diagnosed in the first trimester, noticeably increased amniotic fluid volume between 11–13 weeks may suggest underlying fetal or placental conditions. Early signs are generally picked up in 3D ultrasound research or in cases with associated anomalies.
Sonographic Indicators:
- Excessive separation between fetus and uterine wall.
- Amniotic sac appears overly distended.
- Fetus floating freely in excessive fluid space.
🧾 Possible Causes:
- Fetal gastrointestinal tract anomalies (e.g., esophageal atresia).
- Early neural tube or brain malformations.
- Chromosomal abnormalities (e.g., Trisomy 18 or 21).
- Maternal diabetes (pre-existing or undiagnosed).
- Fetal anemia or cardiac failure (hydrops fetalis).
Management / Follow-Up:
- Repeat scan after 1–2 weeks to monitor AFV trends.
- Targeted early anomaly scan and NT screening.
- First-trimester combined screening (NT, NB, DV, tricuspid flow, PAPP-A, β-hCG).
- Consider referral to fetal medicine unit for high-risk findings.
- Crown-Rump Length (CRL) between 45–84 mm
- Fetal viability confirmed
- Nuchal Translucency (NT)
- Use mid-sagittal view
- Fetal neck in neutral position
➔ NT < 95th percentile ➔ Routine follow-up
➔ NT ≥ 95th percentile (or ≥ 3.5 mm) ➔ HIGH RISK: NIPT / Invasive Testing / Detailed Scan / Echo
- Maternal Age
- Serum Markers (free β-hCG + PAPP-A)
➔ Low Risk ➔ Reassure, Routine Care
➔ High Risk ➔ Genetic Counseling + Diagnostic Testing
Visual Summary
| Step | Action |
|---|---|
| Step-1 | Confirm CRL + Viability |
| Step-2 | Measure NT Accurately |
| Step-3 | Assess NT Thickness |
| Step-4 | Combine with Maternal Serum Markers |
| Step-5 | Calculate Risk (High or Low) |
| Step-6 | Advise NIPT or Invasive Testing if High Risk |
- NT > 3.5mm needs further evaluation.
- Cystic hygroma = much higher risk.
- Normal NT reduces, but doesn't eliminate all risks.
- Combine with Double Marker test for best accuracy!
- Not 100% accurate: NT screening cannot provide a definitive diagnosis.
- Reliability in twins: Less reliable in multiple pregnancies.
- Influence of maternal factors: Obesity, incorrect gestational dating, etc.
- Vanishing Twin Scenario: Can affect NT measurement and results.





































No comments:
Post a Comment