1. Introduction 100%
Role of Ultrasound in Gynecology
Common Indications: AUB, Pain, Infertility, Mass Evaluation
Transabdominal vs Transvaginal Approaches
Advantages and Limitations
Common Indications: AUB, Pain, Infertility, Mass Evaluation
Transabdominal vs Transvaginal Approaches
Advantages and Limitations
2. Uterine Anatomy 100%
Fundus, Body, Isthmus, and Cervix
Endometrial Cavity, Myometrium, Serosa
Junctional Zone (Adenomyosis Marker)
Uterine Arteries and Vascular Supply
Position (Anteverted, Retroverted, Axial)
Endometrial Cavity, Myometrium, Serosa
Junctional Zone (Adenomyosis Marker)
Uterine Arteries and Vascular Supply
Position (Anteverted, Retroverted, Axial)
3. Scanning Techniques 100%
Transvaginal (TVS): High-Resolution, Empty Bladder
Transabdominal (TAS): Full Bladder for Overview
Sagittal and Transverse Planes
Use of Doppler and 3D Ultrasound
Measuring Uterus and Endometrial Thickness
Transabdominal (TAS): Full Bladder for Overview
Sagittal and Transverse Planes
Use of Doppler and 3D Ultrasound
Measuring Uterus and Endometrial Thickness
4. Normal Uterus Appearance 100%
Age-Dependent Uterine Size and Shape
• Endometrial thickness
• Uterine volume
• Uterine wall thickness (UWT)
• LSCS Scar thickness
• Cervical length
• RMT
• Measurement of internal indentation angle
Endometrial Echo: Triple Line, Homogenous, Thickness per Phase
Myometrium: Homogeneous and Isoechoic
Junctional Zone: Intact, Smooth, Hypoechoic
• Endometrial thickness
• Uterine volume
• Uterine wall thickness (UWT)
• LSCS Scar thickness
• Cervical length
• RMT
• Measurement of internal indentation angle
Endometrial Echo: Triple Line, Homogenous, Thickness per Phase
Myometrium: Homogeneous and Isoechoic
Junctional Zone: Intact, Smooth, Hypoechoic
5. Congenital Uterine Anomalies 80%
1. MRKHS/Müllerian duct anomaly
Müllerian duct anomaly -Class-i (Uterine agenesis/uterine hypoplasia)• Class-i-a Vaginal hypoplasia
• Class-i-b Cervical hypoplasia
• Class-i-c Fundal hypoplasia
• Class-i-d Tubal hypoplasia
• Class-i-e combined hypoplasia
Müllerian duct anomaly -Class-ii (Unicornuate Uterus)
• Class-ii-a Unicornuate Uterus (communicating horn)
• Class-ii-b Unicornuate Uterus (Non-communicating horn)
• Class-ii-c Unicornuate Uterus (No cavity)
• Class-ii-d Unicornuate Uterus (No horn)
• Müllerian duct anomaly -Class-iii
Müllerian duct anomaly -Class-iv- (Bicornuate uterus).
• Class-iva (Bicornuate bicollis)
• Class-ivb (Bicornuate unicollis)
• Class-v (septate uterus).
• Class-v-a (Partial/subseptate uterus)
• Class-v-b (Complete septate uterus)
• Class-vi (Arcuate uterus)
2. DES-related T-shaped Uterus
3. Role of 3D US, MRI for Confirmation
6. Myometrial Pathologies 100%
1. Fibroids (Leiomyomas)
2. Adenomyosis
Diffuse AdenomyosisFocal Adenomyosis
Cystic Myometrial Cysts and Striated Pattern
Thickened Junctional Zone >12 mm
7. Endometrial Disorders 100%
Endometrial Hyperplasia
Endometrial Polyp
Endometritis (Acute/Chronic)
Endometrial Carcinoma
Saline Infusion Sonography (SIS) for Cavity Evaluation,br.
Nabothian cyst
Cervicitis
Hematometra
Pyometra
Hematocolpos
Vaginal cyst
Gartner duct cyst
Endometrial Polyp
Endometritis (Acute/Chronic)
Endometrial Carcinoma
Saline Infusion Sonography (SIS) for Cavity Evaluation,br.
Others common findings
Bulky uterusNabothian cyst
Cervicitis
Hematometra
Pyometra
Hematocolpos
Vaginal cyst
Gartner duct cyst
8. Vascular and Functional Disorders 30%
Abnormal Uterine Bleeding (AUB) Evaluation
Arteriovenous Malformation (AVM)
Uterine Synechiae (Asherman’s Syndrome)
Menstrual Phase Correlation with Endometrium
Arteriovenous Malformation (AVM)
Uterine Synechiae (Asherman’s Syndrome)
Menstrual Phase Correlation with Endometrium
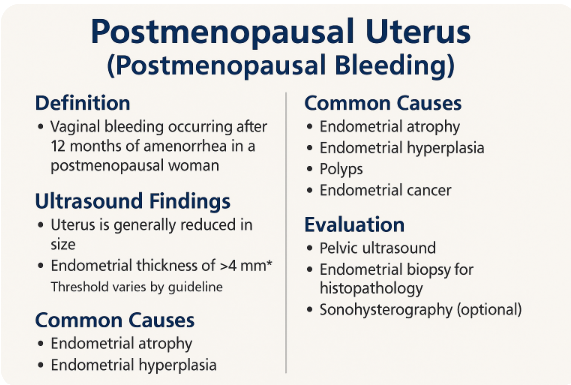
9. Postmenopausal Uterus 0%
Normal Involutional Changes
Endometrial Stripe < 5 mm (Normal)
Postmenopausal Bleeding Evaluation
Endometrial Thickness Guidelines and Biopsy Indications
Endometrial Stripe < 5 mm (Normal)
Postmenopausal Bleeding Evaluation
Endometrial Thickness Guidelines and Biopsy Indications
10. Interventional and Follow-up Role 0%
Hysterosonography (SIS)
US-Guided Fibroid Biopsy
Post-Myomectomy or Hysteroscopic Resection
Treatment Monitoring (GnRH, IUD, Ablation)
US-Guided Fibroid Biopsy
Post-Myomectomy or Hysteroscopic Resection
Treatment Monitoring (GnRH, IUD, Ablation)
11. Case Studies and Quiz Section 0%
Fibroid Localization and Classification
Endometrial Carcinoma vs Hyperplasia Cases
Uterine AVM Diagnosis Challenge
Interactive MCQs with Image Interpretation
Endometrial Carcinoma vs Hyperplasia Cases
Uterine AVM Diagnosis Challenge
Interactive MCQs with Image Interpretation