- Chronic liver disease/cirrhosis (most common background for HCC):
- Hepatitis B virus (HBV) (even without cirrhosis)
- Hepatitis C virus (HCV)
- Alcoholic liver disease
- Non-alcoholic fatty liver disease (NAFLD) / non-alcoholic steatohepatitis (NASH)
- Aflatoxin exposure (contaminated grains, especially in Asia/Africa)
- Genetic conditions:
- Hemochromatosis
- Alpha-1 antitrypsin deficiency
- Wilson’s disease
- Weight loss
- Right upper quadrant abdominal pain
- Jaundice
- Ascites
- Hepatomegaly or a palpable mass
- Decompensation of cirrhosis (new or worsening)
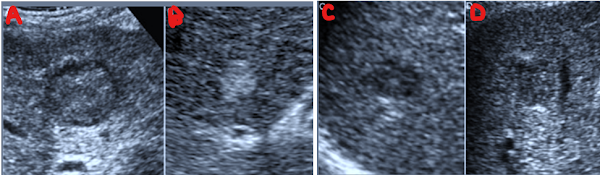
Larger HCCs often display the classic mosaic pattern—different internal densities, occasional halo, and possibly posterior acoustic enhancement
- Hepatocellular carcinoma (HCC)
- Metastases
- Occasionally in benign lesions like hemangiomas or focal nodular hyperplasia, though less commonly.
- Often represents a tumor capsule, compressed liver parenchyma, or inflammatory response.
- In HCC, it may be an indicator of capsular invasion or malignant potential.
1. B-mode (gray-scale) Ultrasound
Large HCC generally appears as a solid, heterogeneous mass—often hypoechoic (darker) or mixed echogenic—and with ill-defined margins.
2. Morphologic Classification
Massive HCC belongs to the “massive” growth type, typically >5 cm, often with necrotic areas and irregular borders.
3. Vascular Features on Doppler/CEUS
Doppler: Chaotic, irregular arterial flow within the tumor (low-resistance waveform).
CEUS:
- Arterial phase (10–30 s): Bright uptake (hyperenhancement) due to abnormal neovascularity.
- Portal/late phase (~60 s): Mild “washout” (relatively hypoechoic), helping differentiate HCC from benign nodules or cholangiocarcinoma.
4. Clinical Context
Massive HCC typically arises in cirrhotic or chronically diseased livers and often presents late, sometimes with vascular invasion or satellite nodules.
| Feature | Description |
|---|---|
| Size & Texture | Large (>5 cm), heterogeneous, often hypoechoic |
| Margin | Irregular, not well demarcated |
| Vascular Behavior | Arterial hyperenhancement → slow, mild washout |
| Typical Context | Cirrhosis or chronic liver disease |
Note: Ultrasound serves as a vital first-line screening tool for liver cancer, complemented by CEUS to characterize suspicious lesions in real-time.
Sonographic Features of Infiltrative HCC
1. Ill‑defined, Geographic Hypoechoic Areas
Rather than a distinct nodule, infiltrative HCC often appears as a diffuse, heterogeneous, hypoechoic region blending into the cirrhotic liver—frequently described as geographic or poorly demarcated.
2. Multiple Small Tumor Foci and Satellite Nodules
Clusters or satellites of small tumor nodules are typically dispersed throughout a hepatic segment or lobe, making the lesion radiologically difficult to discern as a focal mass.
3. Vascular Invasion (Portal Vein Involvement)
Infiltrative HCC often invades vessels, presenting with echogenic tumor thrombus within portal veins, which may demonstrate abnormal flow on Doppler or contrast imaging. Some cases show thrombus extension into the portal system.
4. Contrast‑Enhanced Ultrasound (CEUS) Patterns
- Arterial phase: Early, patchy or geographic hyperenhancement throughout affected segments.
- Portal/late phase: Subtle washout, often less pronounced than in focal HCC, sometimes absent.
Case series images reveal arterial-phase hypervascularity in both the liver parenchyma and tumor thrombus, with subsequent washout.
📋 Summary Table of Infiltrative HCC on Ultrasound
| Feature | Description |
|---|---|
| Echotexture | Geographic, heterogeneous, hypoechoic area |
| Margins | Ill-defined, blending into cirrhotic parenchyma |
| Tumor Nodules | Multiple small foci, often widespread in a segment |
| Vascular Invasion | Portal vein tumor thrombus, echogenic vascular mass |
| CEUS Behavior | Early hyperenhancement, mild-to-moderate washout |
| Detection Difficulty | Easily obscured in cirrhosis due to diffuseness |
Clinical Implications
High index of suspicion is required in cirrhotic patients presenting with new geographic liver changes, rising AFP, or portal vein thrombus. CEUS is especially valuable for real-time visualization of atypical enhancement patterns and early tumor vascularity. Accurate detection demands thorough scanning technique, high-quality imaging equipment, and expert sonographic interpretation.
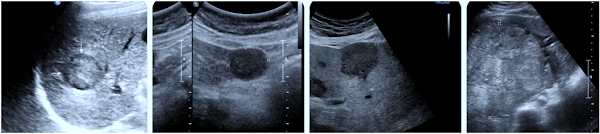 |
| Unifocal HCC: Single lesion. |
| Feature | Description |
|---|---|
| Nodule | Solitary, well-defined |
| Echotexture | Heterogeneous, often hypoechoic (± halo) |
| Size | Usually >2 cm (can be smaller) |
| Vascular invasion | Uncommon in focal type |
| CEUS enhancement pattern | Arterial hyper, portal/late washout |
 |
| Multifocal HCC: Multiple distinct nodules. |
- Demonstrates two well-defined hypoechoic nodules separated by normal tissue—classic multifocal presentation
- Multiple small, heterogeneous hypoechoic to isoechoic lesions scattered across the liver, demonstrating size and echogenic variation
- Larger hypoechoic nodule seen alongside smaller satellite lesions—bi-lobar involvement possible in advanced disease .
- Dense cluster of nodules with varied echotexture; coexisting portal flow abnormalities may suggest vascular invasion .
| USG Feature | Description |
|---|---|
| Nodule pattern | Multiple distinct lesions in one or both lobes |
| Echotexture | Heterogeneous, hypoechoic or mixed |
| Size variability | Nodules of differing sizes; may be satellite clusters |
| Vascular invasion | Possible in larger foci; check portal/hepatic veins |
| CEUS enhancement | Arterial hyperenhancement → portal/late washout |
| Clinical impact | Suggests intermediate/advanced HCC with complex management |
- Strongly dependent on stage at diagnosis and liver function
- Without treatment, median survival may be 6 months.
- With early detection and curative treatment, 5-year survival can exceed 70%.